
Anterior Cruciate Ligament (Acl) Reconstruction
What is it?
It is a procedure that aims to reconstruct the anterior cruciate ligament (ACL), commonly after the native ACL has been ruptured. It is performed arthroscopically, using either the patients’ own tendon tissue (autograft) or donated tendon tissue (allograft). Dr Shiva prefers to use the hamstring tendons as the autograft though there are many other options which differ on a case to case basis.
Most ACL injuries result in complete rupture, but occasionally, the ligament is partially ruptured or grossly stretched. The ACL does not have the ability to heal itself (c.f. collateral ligament), thus patients may contemplate reconstruction. In all of these circumstances, the patient may experience instability of the knee, particularly with cutting and pivoting activities.
ACL injuries are often traumatic events, usually sustained during athletic activity. There may not be pain at the time of injury and a ‘popping’ sound may be heard. Other structures within and around the knee may be injured concomitantly (meniscus, articular cartilage, collateral ligaments) and generally are found concomitantly in a MRI scan and the surgical options for repair are then discussed with you .
Who should have ACL reconstruction surgery?
Patients who have injured/ruptured the ACL and are experiencing instability of the knee during day-to-day activities or during athletic activity are good candidates for the procedure.
It is important to recognise that not everyone needs ACL reconstruction surgery after ACL injury; patients may be able to compensate by good rehabilitation/physiotherapy and the use of a knee brace, depending on the level of athletic activity that the patient wishes to pursue thereafter.
The goals of surgery are to restore normal joint anatomy, to provide static and dynamic stability (and prevent damage to other structures within the knee) and to return to work and sporting activity quickly.
Will I need any tests/scans?
It is likely that X-rays and an MRI will be requested for most knee injuries.
How is it done?
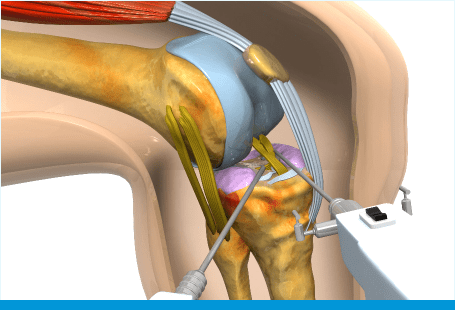
The operation is usually carried out under spinal/ general anaesthetic. If the autograft option has been chosen (more common), then a 2-3cm incision at the upper inner aspect of the shin is made to harvest the hamstring tendons from the thigh. If the allograft option has been chosen, then a small incision in the same place is still made to create the tunnel in the tibia (shinbone) for the new ligament to be fixed into.
Then, the standard knee arthroscopy technique is used to carry out the procedure. Another tunnel is made in the femur (thigh bone) from inside the knee, into which the new ligament will also be passed and fixed. Depending on the graft used, a screw or a sling device is used to hold the graft in place.
At the end of surgery a local anaesthetic is injected into the knee to help minimise post-operative discomfort. Dissolvable stitches are used for the tibial incision and one stitch is used to close each portal. Waterproof dressings are applied. A bandage will be then applied around your knee.
Can I go home the same day?
More often than not, as with most arthroscopic surgery, this is a day case procedure. Occasionally an overnight stay is advised depending on post- operative comfort levels and time of day of the surgery.
What about after the operation?
You will see a physiotherapist before discharge to be instructed on crutch use and simple exercises to carry out in the short term. Crutches are advised for approximately 2-4 weeks, but this varies from patient to patient.
You will be allowed to weight-bear as tolerated in most cases. Swelling of the knee and lower leg and bruising is very common after ACL reconstruction and to be expected. It may persist for several weeks until full range of motion and mobility has been regained.
You will be prescribed analgesia to take home.
You will see Dr shiva two weeks after surgery for a wound check (and stitch removal) and a physiotherapy program will ensue thereafter which is paramount to the success of the operation. You are likely to have been seeing a physiotherapist before the operation and Dr shiva will liaise with him/her in detail to advise on the post-operative exercise program.
Each individual recovers and rehabilitates at a different pace; as an approximation, Dr Shiva recommends that you do not return to full activity/sport before 6 months after first time ACL reconstruction. The use of allograft may extend this recovery period.
What are the potential complications?
All surgery carries a risk. Specific risks to ACL reconstruction are:
Infection – this can be either superficial (portals) or within the joint. The latter may necessitate removal of all metalwork and the graft to eradicate the infection completely. The operation can be repeated once the infection has been cleared. You will be given antibiotics to reduce this risk.
Thrombosis – a clot in the deep veins of the lower limb. The risk is minimised by early mobility if possible. Oral contraceptive pills and HRT, which are known to increase risk, should be stopped before surgery.
Bleeding – this may require a return to the operating room for removal of blood clots and to stop the bleeding.
Stiffness – It is very important that some mobility of the knee is maintained after surgery. The physiotherapist will advise on simple exercises that can be carried out at home. It is also recommended that you take regular analgesia and apply ice to help minimise post- operative discomfort and facilitate early movements.
Re-rupture/injury – The reconstructed ACL ligament is not infallible and can be re-ruptured by similar mechanisms to rupture of the native ACL.
Neurological symptoms – occasionally, patients may experience a patch of numbness on the inner aspect of the shin; this is related to the process of hamstring tendon harvest and associated swelling within the thigh. It is often temporary and resolves spontaneously after several weeks.
Residual symptoms – ACL reconstruction has a high success rate (>90%) in terms of stabilising the knee joint for athletic activity. However, unfortunately, no guarantees can be offered regarding curing your symptoms, despite the surgeon’s best efforts. In this case, further management and treatment options will be discussed with you.
